Gestational Diabetes Education
As an Amazon Associate I earn from qualifying purchases.
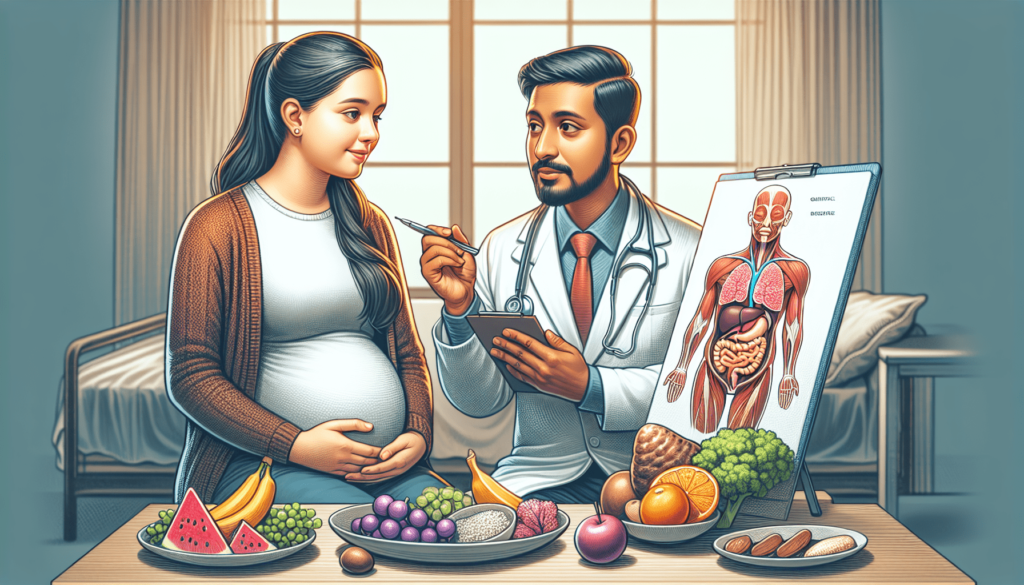
Imagine being pregnant and learning that you have gestational diabetes. It can feel overwhelming and confusing, but don’t worry – help is here. In this article, we will guide you through the world of gestational diabetes education, providing you with valuable information and resources to help you manage your condition and have a healthy pregnancy. Whether you’re looking for tips on nutrition, exercise, or monitoring your blood sugar levels, we’ve got you covered. So sit back, relax, and let’s embark on this educational journey together.
What is Gestational Diabetes?
Definition and Explanation
Gestational diabetes is a condition that affects pregnant women and is characterized by high blood sugar levels. It occurs when the body is unable to produce or properly use insulin, a hormone that helps regulate blood sugar. Unlike other types of diabetes, gestational diabetes typically resolves after giving birth. However, women who have gestational diabetes are at a higher risk of developing type 2 diabetes later in life.
Causes and Risk Factors
The exact cause of gestational diabetes is not fully understood. However, it is believed to be a combination of hormonal changes and insulin resistance during pregnancy. Hormones produced by the placenta can inhibit the action of insulin, resulting in elevated blood sugar levels. Certain risk factors increase the likelihood of developing gestational diabetes, including being overweight or obese, having a family history of diabetes, being older than 25, and having previously given birth to a large baby.
Diagnosis of Gestational Diabetes
Screening Tests
Gestational diabetes is typically diagnosed between the 24th and 28th week of pregnancy. The initial screening test, known as the glucose challenge test, involves drinking a sweet liquid and having blood drawn to measure blood sugar levels. If the results of the screening test are above a certain threshold, further testing is required to confirm the diagnosis.
Oral Glucose Tolerance Test
The oral glucose tolerance test is the gold standard for diagnosing gestational diabetes. During this test, pregnant women fast overnight and then have their blood sugar levels measured. They are then given a sugar solution to drink, and their blood sugar levels are checked at regular intervals over the next few hours. If blood sugar levels are elevated beyond the acceptable range, a diagnosis of gestational diabetes is made.
Criteria for Diagnosis
The criteria for diagnosing gestational diabetes vary depending on the specific guidelines followed by healthcare professionals. However, commonly used criteria include a fasting blood sugar level of 92 mg/dL or higher, a one-hour blood sugar level of 180 mg/dL or higher, or a two-hour blood sugar level of 153 mg/dL or higher.
Risk and Complications
Risks to Mother and Baby
Untreated gestational diabetes can pose risks to both the mother and the baby. For the mother, gestational diabetes increases the risk of developing preeclampsia, a condition characterized by high blood pressure, as well as the need for a cesarean delivery. It also increases the likelihood of developing type 2 diabetes later in life. For the baby, gestational diabetes increases the risk of macrosomia, or a large birth weight, which can lead to difficulties during delivery. It also increases the risk of hypoglycemia (low blood sugar) and respiratory distress syndrome in the newborn.
Long-Term Health Effects
While gestational diabetes typically resolves after pregnancy, it is important to recognize that having gestational diabetes can have long-term health effects for both the mother and the child. Women who have had gestational diabetes are at a higher risk of developing type 2 diabetes later in life. Additionally, children born to mothers with gestational diabetes have an increased risk of obesity and developing type 2 diabetes themselves.

Managing Gestational Diabetes
Importance of Blood Sugar Control
Managing gestational diabetes is crucial for the health of both the mother and the baby. By controlling blood sugar levels, the risk of complications can be minimized. This involves working closely with healthcare professionals and following their recommendations for lifestyle changes, monitoring blood sugar levels, and potentially taking medications or insulin if necessary.
Diet and Nutrition
Diet plays a key role in managing gestational diabetes. It is important to consume a balanced diet that includes a variety of nutrient-rich foods. Carbohydrate counting is commonly recommended to help manage blood sugar levels. This involves monitoring the amount of carbohydrates consumed and spreading them evenly throughout meals and snacks. Portion control is also important to prevent excessive blood sugar spikes.
Physical Activity
Regular physical activity is beneficial for managing gestational diabetes. It helps lower blood sugar levels and can improve insulin sensitivity. However, it is important to engage in safe exercises that are suitable for pregnancy. Low-impact activities such as walking, swimming, and prenatal yoga are generally considered safe options. It is recommended to consult with healthcare professionals before starting or modifying an exercise routine.
Monitoring Blood Sugar Levels
Regularly monitoring blood sugar levels is essential for managing gestational diabetes. This can be done through self-monitoring using a glucose meter. Typically, healthcare professionals will provide specific instructions on when and how often to test blood sugar levels, as well as target ranges to aim for.
Medications and Insulin Therapy
In some cases, lifestyle modifications alone may not be sufficient to control blood sugar levels in women with gestational diabetes. Medications or insulin therapy may be prescribed to help regulate blood sugar. Oral medications, such as metformin, can be used to lower blood sugar levels. In more severe cases, insulin injections may be necessary. It is important to closely follow healthcare professionals’ instructions and regularly monitor blood sugar levels when using medications or insulin.
Blood Sugar Monitoring
Methods of Monitoring
Blood sugar levels can be monitored using a glucose meter or continuous glucose monitoring (CGM) system. A glucose meter requires a small blood sample obtained by pricking the finger with a lancet. The blood sample is then applied to a test strip, and the meter displays the blood sugar level. CGM systems use a small sensor inserted under the skin, which continuously measures glucose levels and displays them on a device or smartphone app.
Frequency and Timing
Healthcare professionals will provide specific instructions on how often to monitor blood sugar levels. Generally, this involves testing upon waking in the morning (fasting), before meals, and one to two hours after meals. Additional monitoring might be required during times of illness or changes in medication or lifestyle.
Interpreting Results
Interpreting blood sugar level results is essential for managing gestational diabetes. Target ranges for blood sugar levels can vary depending on the healthcare professional’s recommendations. Typically, fasting blood sugar levels should be between 70-95 mg/dL, while post-meal levels should be below 130 mg/dL one hour after a meal or below 120 mg/dL two hours after.
Healthy Eating Habits
Balanced Diet During Pregnancy
Maintaining a balanced diet is crucial for overall health during pregnancy, and even more so when managing gestational diabetes. It is important to consume a variety of nutrient-dense foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Avoiding processed foods, sugary beverages, and excessive sweets can help control blood sugar levels.
Carbohydrate Counting
Carbohydrate counting is a method used to plan meals and manage blood sugar levels in people with diabetes, including gestational diabetes. It involves keeping track of the amount of carbohydrates consumed in each meal and adjusting portion sizes accordingly. Healthcare professionals can provide guidance on how many carbohydrates to consume at each meal and snack to maintain balanced blood sugar levels.
Meal Planning and Portion Control
Meal planning can be a helpful tool for managing gestational diabetes. Planning meals in advance, including healthy snack options, can ensure a balanced intake of nutrients and help control blood sugar levels. Portion control is also important and can be achieved by measuring or estimating serving sizes and avoiding oversized portions.
Physical Activity and Exercise
Benefits of Exercise
Engaging in regular physical activity has numerous benefits for both the mother and the baby during pregnancy. Exercise can help control blood sugar levels, improve energy levels, reduce pregnancy discomfort, promote healthy weight gain, and enhance overall well-being. It is important to choose safe exercises that are suitable for pregnancy to minimize the risk of injury.
Safe Exercises During Pregnancy
Low-impact exercises are generally considered safe for pregnant women with gestational diabetes. Walking, swimming, stationary biking, prenatal yoga, and low-impact aerobics are commonly recommended. It is important to listen to your body, avoid exercises that cause discomfort or pain, and consult with healthcare professionals before starting any new exercise program.
Scheduling and Duration
Finding a balance between rest and physical activity is important during pregnancy. Aim for at least 150 minutes of moderate-intensity exercise spread throughout the week. Breaking it down into shorter sessions or incorporating activities into daily routines can make it more manageable. Be sure to schedule exercise at times that work best for you and your energy levels.
Medications and Insulin Therapy
Oral Medications
In some cases, lifestyle modifications alone may not be sufficient to control blood sugar levels in women with gestational diabetes. When necessary, oral medications may be prescribed to help regulate blood sugar levels. Metformin is a commonly used oral medication that can help lower blood sugar levels. It is important to strictly follow healthcare professionals’ instructions and regularly monitor blood sugar levels when taking medications.
Insulin Injections
If blood sugar levels remain uncontrolled with oral medications or if the severity of gestational diabetes calls for immediate management, insulin therapy may be recommended. Insulin injections help regulate blood sugar levels by providing the body with the necessary insulin it may be lacking. Insulin therapy requires careful monitoring and close communication with healthcare professionals to ensure proper dosing and to prevent complications.
Safety Considerations
When using medications or insulin therapy, it is important to be aware of potential side effects or risks. Some medications may cause gastrointestinal discomfort or other adverse effects. Insulin therapy requires proper storage and handling to maintain its effectiveness. Safety precautions should be taken, and any concerns or questions should be discussed with healthcare professionals.
Birth and Postpartum Considerations
Delivery Options
Women with gestational diabetes have the same delivery options as women without gestational diabetes. The choice of delivery method depends on various factors, such as blood sugar control, the size and health of the baby, and any complications that may arise during pregnancy. Vaginal delivery is often the preferred option, but in some cases, a cesarean delivery may be necessary.
Monitoring Blood Sugar After Birth
After giving birth, blood sugar levels typically return to normal. However, healthcare professionals may continue to monitor blood sugar levels for a period of time to ensure they remain stable. It is important to follow any postpartum monitoring guidelines provided by healthcare professionals.
Breastfeeding and Lactation
Breastfeeding is generally encouraged for women with gestational diabetes, as it provides numerous benefits for both the mother and the baby. Breastfeeding can help regulate blood sugar levels in the mother and provide optimal nutrition for the baby. However, it is important to work closely with healthcare professionals to ensure blood sugar levels remain stable while breastfeeding.
Support and Follow-up Care
Importance of Healthcare Team
Managing gestational diabetes involves a multidisciplinary approach that includes healthcare professionals from various fields. This team may include obstetricians, endocrinologists, dietitians, nurses, and diabetes educators. Regular communication and collaboration with the healthcare team are essential for optimal management and support throughout the pregnancy and beyond.
Monitoring and Tracking Progress
Regular follow-up appointments and monitoring are essential for tracking the progress of gestational diabetes management. Healthcare professionals will assess blood sugar levels, discuss any concerns or questions, make necessary adjustments to the treatment plan, and provide guidance on maintaining a healthy lifestyle. Keeping a record of blood sugar levels, meals, exercise, and medications can be helpful during follow-up appointments.
Lifestyle Changes for Long-Term Health
While gestational diabetes typically resolves after giving birth, it is important to recognize that having gestational diabetes increases the risk of developing type 2 diabetes later in life. Making permanent lifestyle changes, such as adopting healthy eating habits, engaging in regular physical activity, and maintaining a healthy weight, can reduce the risk of developing type 2 diabetes and improve overall long-term health.
In conclusion, gestational diabetes is a condition that requires careful management to ensure the well-being of both the mother and the baby. By working closely with healthcare professionals, monitoring blood sugar levels, following a balanced diet, engaging in safe physical activity, and, if necessary, taking medications or insulin, women with gestational diabetes can successfully manage the condition and minimize the risk of complications. With proper support and follow-up care, women can make lifestyle changes that promote long-term health and reduce the risk of developing type 2 diabetes.
Amazon and the Amazon logo are trademarks of Amazon.com, Inc, or its affiliates.